Topical Intranasal Anesthetics
Introduction
A plethora of data demonstrates the efficacy and importance of topic anesthesia prior to procedural manipulation of the nose, throat and upper airway.[1-21] However, local anesthetics used in improper doses can lead to toxic effects on the cardiovascular and central nervous systems as well as methemoglobinemia. Furthermore, there is a large number of topically active anesthetics and multiple methods of delivering these medications. All these choices and variable procedures may cause confusion - there is still a wide variation in the use of topical anesthetics before many oropharyngeal and laryngotracheal procedures.
Due to this variable practice and the concern of medication toxicity, the National Center for Patient Safety joined forces with the Veterans Hospital Association and created a set of recommendations on this topic. This document was published in 2006 and is titled: A guidance on the Use of Topical Anesthetic for Naso/oropharyngeal and Laryngotracheal procedures.
Because this is such a recent review that covers the topic in great depth, and because it is free to the public, we have elected to not add additional material on the subject. Please simply refer to the web site link below for the most recent update or review the article posted on this web site.
Literature overview:
A guidance on the use of topical anesthetic for nasal/oropharyngeal and laryngotracheal procedures:
Full PDF document from national center for patient safety (click here)
The FDA also has a web site that tracks safety issues related to topical anesthetics - specifically methemoglobinemia related to benzocaine use. This web link can be accessed here:
FDA Safety Alert - Benzocaine induced methemoglobinemia
Since the time of the above patient safety publication, multiple newer studies have been published. One of the more compelling studies was for reducing pain during NG tube placement. This study by Chan et al looked at 206 patients randomized to topical nasal and oral lidocaine versus placebo. They found dramatic differences in pain scores, ease of NG tube placement and success at placement if the patient was pretreated with topical lidocaine (and enough time was allowed to elapse for it to be effective - i.e. do not be in too big of a hurry as it takes time for topical anesthetics to take effect). The following graph demonstrates their results:
You can read the entire article by clicking here: Chan, Lidocaine spray for NGT, Hong Kong Med J 2010.pdf
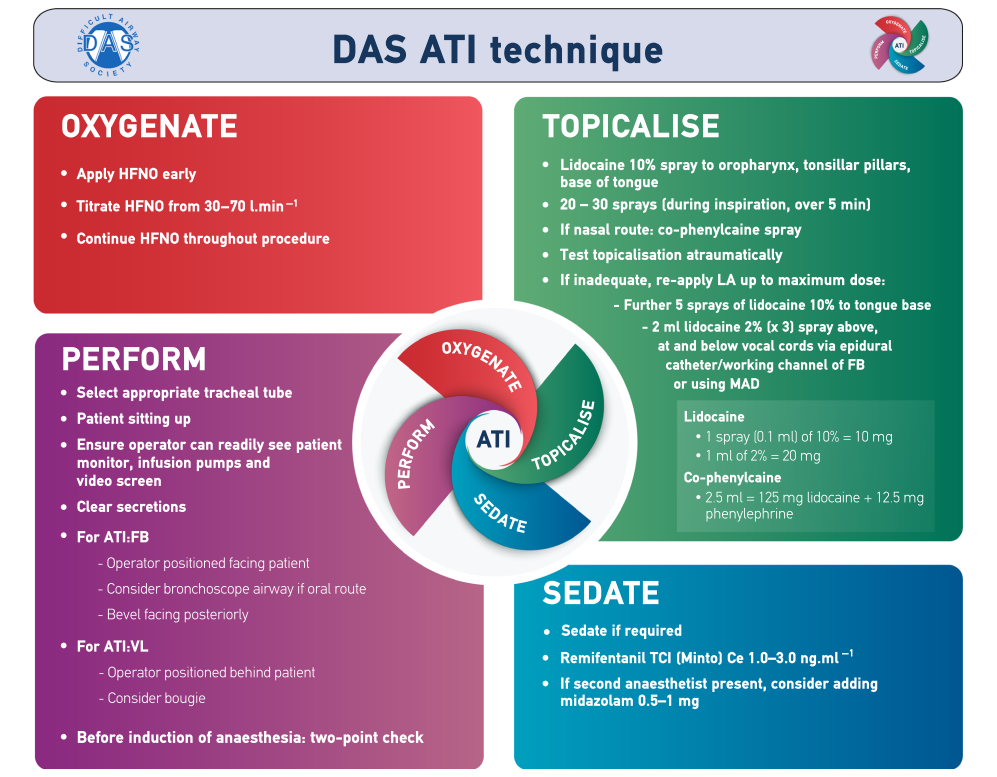
Another compelling publication on the topic is the latest (2020) difficult airway society guidelines for awake intubation.[23] A central concept to their guidelines in topical anesthetic application. They incorporate topical lidocaine into the algorithm using a technique similar to that described below for nasopharyngeal procedures. They are a British organization so use forms of lidocaine not necessarily available to everyone but the concept is the same. You can download their guidelines for free from the internet - click here for the document. Here is the graphic from their free guidelines:
In contrast to these findings for sprayed lidocaine, nebulized lidocaine is relatively ineffective and time consuming. Babl et al actually showed nebulized lidocaine to cause distress and not reduce pain associated with NGT placement in children.[22] (In the opinion of the web site authors, the most likely cause for nebulized drugs to be ineffective when compared to nasal and buccal delivery is that most of the medication is lost into the environment and never even gets to the patient. furthermore it takes considerable time to deliver so the clinical effect is delayed.)
Treatment Protocol
NASOPHARYNGEAL PROCEDURES: NASAL AND ORAL 4% LIDOCAINE (with or without oxymetazoline)
Indications: To reduce pain and gagging
and induce vasoconstriction in patients requiring:
- Nasogastric tubes
- Nasal intubations
- Nasal fiberoptic procedures
Alternate Indication: As an option to treat selected migraine, cluster or ice pick temporal headaches by blocking the sphenopalatine ganglion in the nasal cavity
- Load a 5cc syringe with 4.5 ml of 4% lidocaine
and attach nasal atomizer (adult dose)
- A topical vasoconstrictor such as oxymetazoline can also be used either as a separate spray or mixed with the lidocaine to shrink mucosal membranes and constrict blood vessels. This will reduce risk of epistaxis during the procedure and open the nasal cavity to allow easier passage of the device.
- Give the patient a tissue to capture any runoff solution
- Place atomizer within the selected nostril
- Briskly compress syringe to administer 1.5 ml of atomized spray into the nose. If the patient is awake, ask them to inhale through their nose during the time you spray.
- Remove atomizer from the nostril and open the patient’s mouth. Spray the remaining 3 ml of 4% lidocaine into throat. If the patient is awake, ask them to gargle and swallow. (Oral lidocaine not needed to treat headaches)
- Lubricate end of NGT or ETT.
- Squirt lidocaine jelly or viscous lidocaine into nostril using syringe or nasal atomizer (it will come out as a stream) to further anesthetize the nose.
- After the lidocaine has had 3-5 minutes to take effect, insert the device as per standard protocol. If anesthesia is inadequate, repeat with ½ dose and allow several more minutes to take effect.
Topical Lidocaine dosing protocol
Indication: Topical anesthetics are partially absorbed into the blood stream and if high doses result may lead to cardiovascular (arrhythmias) and neurologic (seizures) toxicity. Lidocaine is one of the safer topical anesthetics but can still lead to these complications if improperly applied. To prevent the risk of these toxic side effects, it is important to limit the volume of topically applied lidocaine to doses well within the safety range.
Dose: A reasonable dose that is safe
for topical lidocaine is 4 mg/kg. (Doses as high as 7 mg/kg
may be considered safe if a topical vasoconstrictor (oxymetazoline) is
applied prior or simultaneously to the lidocaine.)
|
Comments:
- When performing a nasal procedure, strongly consider a topical vasoconstrictor in addition to the lidocaine to prevent bleeding and shrink the nasal mucosa. This can be mixed with the lidocaine or applied separately. Oxymetazoline probably has best safety profile in children.
- When possible allow a full 3-5 minutes for lidocaine to take complete effect before performing the procedure.
Teaching materials
Chan, Lidocaine spray prior to NG tube placement, Hong Kong Med Journal 2010
Links
FDA Safety Alert - Benzocaine induced methemoglobinemia
Bibliography (click here for abstracts)
1. Stolz, D., et al., Nebulized lidocaine for flexible bronchoscopy: a randomized, double-blind, placebo-controlled trial. Chest, 2005. 128(3): p. 1756-60.
2. Korttila, K., Local anesthetic techniques for bronchoscopies. Acta Anaesthesiol Belg, 1984. 35 Suppl: p. 389-97.
3. Ristikankare, M., et al., Is routine sedation or topical pharyngeal anesthesia beneficial during upper endoscopy? Gastrointest Endosc, 2004. 60(5): p. 686-94.
4. Hedenbro, J.L., et al., A randomized, double-blind, placebo-controlled study to evaluate topical anaesthesia of the pharynx in upper gastrointestinal endoscopy. Endoscopy, 1992. 24(6): p. 585-7.
5. Gordon, M.J., G.R. Mayes, and G.W. Meyer, Topical lidocaine in preendoscopic medication. Gastroenterology, 1976. 71(4): p. 564-9.
6. Mulcahy, H.E., et al., A double-blind randomized trial of low-dose versus high-dose topical anaesthesia in unsedated upper gastrointestinal endoscopy. Aliment Pharmacol Ther, 1996. 10(6): p. 975-9.
7. Dhir, V., et al., Topical pharyngeal anesthesia without intravenous sedation during upper gastrointestinal endoscopy. Indian J Gastroenterol, 1997. 16(1): p. 10-1.
8. Jameson, J.S., et al., Is oropharyngeal anaesthesia with topical lignocaine useful in upper gastrointestinal endoscopy? Aliment Pharmacol Ther, 1992. 6(6): p. 739-44.
9. Williams, K.A., et al., Combined nebulization and spray-as-you-go topical local anaesthesia of the airway. Br J Anaesth, 2005. 95(4): p. 549-53.
10. Sutherland, A.D. and J.P. Sale, Fibreoptic awake intubation--a method of topical anaesthesia and orotracheal intubation. Can Anaesth Soc J, 1986. 33(4): p. 502-4.
11. Stoelting, R.K., Circulatory response to laryngoscopy and tracheal intubation with or without prior oropharyngeal viscous lidocaine. Anesth Analg, 1977. 56(5): p. 618-21.
12. Venus, B., V. Polassani, and C.G. Pham, Effects of aerosolized lidocaine on circulatory responses to laryngoscopy and tracheal intubation. Crit Care Med, 1984. 12(4): p. 391-4.
13. Frosh, A.C., et al., Is local anaesthesia actually beneficial in flexible fibreoptic nasendoscopy? Clin Otolaryngol Allied Sci, 1998. 23(3): p. 259-62.
14. Cullen, L., et al., Nebulized lidocaine decreases the discomfort of nasogastric tube insertion: a randomized, double-blind trial. Ann Emerg Med, 2004. 44(2): p. 131-7.
15. Wolfe, T.R., D.E. Fosnocht, and M.S. Linscott, Atomized lidocaine as topical anesthesia for nasogastric tube placement: A randomized, double-blind, placebo-controlled trial. Ann Emerg Med, 2000. 35(5): p. 421-5.
16. Ducharme, J. and K. Matheson, What is the best topical anesthetic for nasogastric insertion? A comparison of lidocaine gel, lidocaine spray, and atomized cocaine. J Emerg Nurs, 2003. 29(5): p. 427-30.
17. Mainland, P.A., et al., Absorption of lidocaine during aspiration anesthesia of the airway. J Clin Anesth, 2001. 13(6): p. 440-6.
18. Graham, D.R., et al., Comparison of three different methods used to achieve local anesthesia for fiberoptic bronchoscopy. Chest, 1992. 102(3): p. 704-7.
19. Middleton, R.M., A. Shah, and M.B. Kirkpatrick, Topical nasal anesthesia for flexible bronchoscopy. A comparison of four methods in normal subjects and in patients undergoing transnasal bronchoscopy. Chest, 1991. 99(5): p. 1093-6.
20. Groeben, H., et al., Lidocaine inhalation for local anaesthesia and attenuation of bronchial hyper-reactivity with least airway irritation. Effect of three different dose regimens. Eur J Anaesthesiol, 2000. 17(11): p. 672-9.
21. Sitzman, B.T., et al., Local anesthetic administration for awake direct laryngoscopy. Are glossopharyngeal nerve blocks superior? Anesthesiology, 1997. 86(1): p. 34-40.
22.
Babl, F.E., et al., Does nebulized
lidocaine reduce the pain and distress of nasogastric tube insertion in
young children? A randomized, double-blind, placebo-controlled trial.
Pediatrics, 2009. 123(6): p.
1548-55.
 Therapeutic
Intranasal Drug Delivery
Therapeutic
Intranasal Drug Delivery